New way of defining Alzheimer's aims to find disease sooner
Government and other scientists are proposing a new way to define Alzheimer's disease.
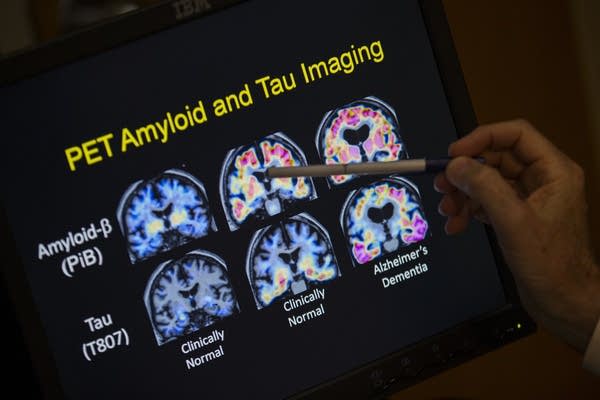
Evan Vucci | AP 2015
Go Deeper.
Create an account or log in to save stories.
Like this?
Thanks for liking this story! We have added it to a list of your favorite stories.


