COVID steady, RSV and flu down, but hospitals still packed tight

Go Deeper.
Create an account or log in to save stories.
Like this?
Thanks for liking this story! We have added it to a list of your favorite stories.
Last week the CDC reported a 49.6 percent increase in average new daily cases of COVID-19—the largest such increase since last January, when the nation was in the grips of the initial omicron surge. On the eve of holiday gatherings, this raised the specter of another such wave—and was followed by the White House announcement that Americans can once again order free COVID tests.
Fortunately, this week’s national data shows a three percent drop in COVID cases. While this does not at all suggest that last week’s concerns were misplaced—especially in light of continued pressures on the nation’s hospitals due to the so-called “tripledemic” of COVID, RSV and the flu—the leveling off is welcome.
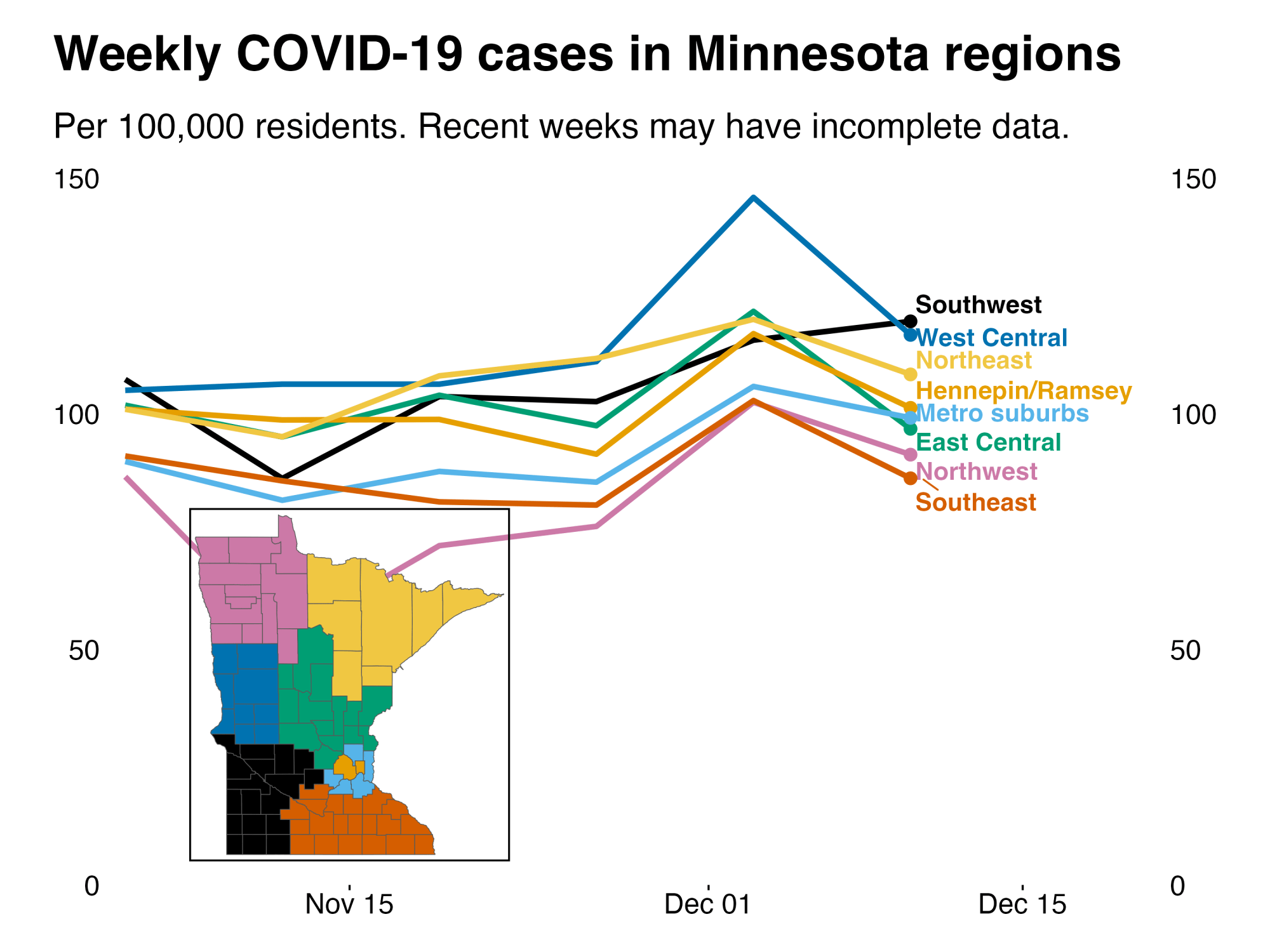
Here in Minnesota, the weekly case rates were up slightly more than the national rates last week (57 percent), and this week they are down much more (-23 percent). The state’s weekly case rate, which has mirrored national rates since mid-September, currently stands at 105 per 100,000, compared with 137 per 100,000 nationally.
Of course, case rates are only part of the picture, and probably not even the best measure we have. For a more complete rundown of the latest data, read on. And at the end of today’s update, new data on deaths due in part to long COVID, including a specific look at Minnesota.
Turn Up Your Support
MPR News helps you turn down the noise and build shared understanding. Turn up your support for this public resource and keep trusted journalism accessible to all.
COVID-19 cases and hospitalizations down, RSV easing, but hospital bed usage still high
Last week’s jump in cases across the state has for the most part reversed in this week's data. Cases went up again in southwestern Minnesota, but in all other regions, cases fell. And in many parts of the state, cases went back to levels seen two weeks ago or lower. So the post-Thanksgiving bump hasn't yet translated into a full-blown COVID surge.
Non-intensive care COVID hospitalizations followed a similar trend recently. After jumping up to the highest level since early 2022, non-ICU hospitalizations declined in the past week of data.
Intensive care unit COVID admissions have been jumping around but, on the whole, have been increasing since early October. Most recent average ICU admissions have been around 12 per day statewide. While lower than past years at this time, that average is four times higher than the low point for this year – the last week of March 2022, when we saw three admissions per day.

Hospitalizations from RSV and flu continue to be a concern, although RSV hospitalizations have now fallen for several weeks in a row. Flu hospitalizations stayed approximately level for two weeks in a row, and the most recent week of data suggests those may be falling as well, although delays in data reporting make it difficult to say for sure. Flu came earlier this year, and it’s not yet known if flu cases will peak early and drop off, or stay elevated.
Despite the signals that seasonal viruses may be easing, hospitals remain strained. Last week, we showed hospital bed use for non-ICU beds, for both adults and children. Those rates remain relatively the same this week for adults and have dropped a couple of percentage points for children. Pediatric ICU bed usage is also down a few percentage points. Last week, there were four pediatric ICU beds available in Minnesota. This week, that number has gone up to seven beds available.
The category of bed usage that did increase this week was adult ICU beds in Greater Minnesota. After staying relatively stable since spring 2022, adult ICU bed usage has recently jumped a few percentage points in Greater Minnesota.

The recent jump in COVID hospitalizations has not yet translated into a corresponding jump in COVID deaths, as we have sometimes seen. It’s possible, however, that counts of deaths for recent weeks could still be revised upwards as data comes in.

COVID-19 levels (and variants) measured in Minnesota’s wastewater remain concerning
The most recent wastewater analysis in the state, from the Metropolitan Council and the University of Minnesota’s Genomic Center, shows COVID levels unchanged for the week ending Dec. 12, as compared to the week prior. The current levels, however, remain about 65 percent higher than measured one month ago.
The prevalence of COVID-19 RNA is now the highest seen in the Metro plant since July. It remains much lower than it was during last December’s delta surge, but almost identical to measurements taken in December 2020 on the downswing of the earlier surge that fall.

Perhaps as concerning as the continued elevated COVID levels is the continued rise in the new BQ.1 subvariant. New strains have led to surges of COVID-19 in the past. While the data are not yet suggesting that to be the case here in Minnesota, it may be the introduction of new subvariants are preventing the declines in COVID infections that we would all like to see.

The latest data out of the University of Minnesota’s Wastewater SARS-CoV2 Surveillance Study, which tracked data from seven regions through Dec. 4, again shows a general increase in COVID-19 levels across most of the state, over both the prior month and week.
The North West region of the study, which samples from wastewater plants in Beltrami, Clay and Pennington counties, shows the most concerning monthly and weekly increases—although the COVID levels measured at those plants were quite low in November.
CDC is again encouraging masking to help prevent spread of respiratory diseases, even while zero Minnesota counties are rated as having “high” community levels
Last week CDC Director Dr. Rochelle Walensky encouraged Americans to consider masking to help address the spread of COVID-19, RSV and the flu, stating: “We also encourage you to wear a high quality, well-fitting mask to prevent the spread of respiratory illnesses, most especially for those in the 5% of the population currently living in counties with high COVID-19 community level. CDC continues to recommend masking for anyone choosing to travel by plane, train, bus or other form of public transportation, or for anyone who may be immunocompromised or increased risk of severe disease.”
This week’s CDC map of COVID-19 community levels shows zero Minnesota counties rated as high, a welcome decrease from the five counties rated in that danger zone last week. Thirty-three counties are rated medium.
As is often the case, the CDC’s community level ratings (above) seem more rosy than their “COVID-19 transmission” ratings. Those ratings show 44 Minnesota counties as having “high transmission,” exceeding the CDC’s threshold of 100 cases per 100,000. This includes four counties where case rates exceed 200 per 100,000: Big Stone, Chippewa, Stevens and Lac qui Parle.
CDC releases long COVID mortality study; Muckrock looks at Minnesota long COVID deaths
This week the CDC released a report finding that long COVID-19 contributed to at least 3,544 deaths from Jan. 1, 2020 to June 30, 2022. Journalists at Muckrock used similar methods to identify such deaths, including 62 in Minnesota, with data they received from records requests in a handful of jurisdictions.
These estimates are likely an undercount, as clinical guidance around documenting long-COVID or post-COVID conditions has evolved over time and is not necessarily uniform across the medical community. In Minnesota, more than half of the estimated long COVID deaths were people who were at least 80 years old, and 50 of the 62 deaths were people aged 70 or older. Deaths were reported from residents of 36 of the state’s 87 counties, with Hennepin reporting the most (12) and Washington the second-most (5).
Long COVID death estimates likely skew older and whiter. Younger people may be less likely to be counted because the link to COVID with their primary cause of death, such as heart complications, might be less obvious than for older people who have continuing respiratory conditions following a COVID infection.
David Putrino, an expert in rehabilitation medicine at Mount Sinai, told Muckrock that a doctor might also be more likely to diagnose long COVID in people who had more severe acute COVID systems, which would also tend to bias the data older. Putrino also said that white people are more likely to have doctors that are educated in long COVID, as thus more likely to make that diagnosis or enter it on medical records.
Given these limitations, the Minnesota data is probably not a perfect representation of all people who have died with lingering COVID symptoms playing a role. But Muckrock made it available publicly here should you wish to dig in.
Even with imperfect data that doesn’t represent the full impact of long COVID on mortality, researchers told Muckrock there should be more public warnings about the cardiovascular risks following COVID infection, as well as links to other chronic conditions.
If you are experiencing persistent, new or changing post-COVID symptoms, the Pan American Health Organization suggests contacting your doctor or otherwise seeking medical care. If those symptoms include sudden and severe shortness of breath, chest pain, suicidal thoughts, coughing up blood, severe headache or weakness on one side of the body and slurred speech, PAHO suggests seeking care immediately.


